The unseen epidemic: Urgent global push to halt tobacco’s deadly toll on the mentally ill
12/15/2025 / By Ava Grace

- People with mental health conditions are three times more likely to smoke, losing 15–20 years of life, creating an “unseen epidemic” of tobacco-related death.
- A mistaken belief that quitting smoking is futile or harmful for this group has led to systemic neglect and a widening life-expectancy gap.
- This population consumes 44% of cigarettes in Western nations, with the crisis being especially acute in low- and middle-income countries where support is scarce.
- The SCIMITAR+ trial proved that a tailored smoking cessation program is both safe and effective for people with mental illness, without disrupting their mental health.
- Success requires integrating cessation into mental health care, training professionals and ensuring policies and affordable aids reach this vulnerable group.
In a stark call to action, a leading researcher has declared an “unseen epidemic” of tobacco-related deaths ravaging a vulnerable global population: people living with mental health conditions. Professor Simon Gilbody of the University of York, writing with colleagues in the prestigious New England Journal of Medicine, is demanding urgent international intervention to address a staggering health inequity.
The facts are chilling: Individuals with depression, schizophrenia, or bipolar disorder are about three times more likely to smoke than the general public, shaving 15 to 20 years off their lives. This crisis, long overlooked within fragmented health systems, now has a proven solution, and the time for its global implementation is now.
A historical blind spot in care
For decades, the profound physical health decline of those with mental illness has been a tragic constant in medicine worldwide. While attention focused on psychiatric symptoms, a parallel crisis of cardiovascular disease, cancer and respiratory illness—largely driven by tobacco use—went unaddressed. A pervasive sense of therapeutic nihilism, the belief that helping these patients quit was futile or even harmful, became a barrier to care. Smoking was often incorrectly viewed as an inevitable coping mechanism and fears that cessation would destabilize mental health led to a deadly inertia. This neglect has created a widening gap in life expectancy, a direct contradiction to the duty of care.
The statistics underscore a global emergency. People with mental health conditions consume a disproportionate 44% of all cigarettes in Western nations. The problem is even more acute in low- and middle-income countries, which are home to nearly 80% of the world’s tobacco users and face high burdens of mental illness. In these regions, mental health often receives less than 2% of total health expenditures, and cessation medications are frequently unavailable or unaffordable. The result is a perfect storm where cheap tobacco products and minimal support converge on a population already facing significant challenges.
A blueprint for success: The SCIMITAR+ trial
The cornerstone of Professor Gilbody’s argument is hard evidence that shatters old myths. The SCIMITAR+ trial (Smoking Cessation Intervention for severe Mental Ill Health Trial), the largest study of its kind, tested a tailored smoking cessation program specifically designed for people with mental ill health. Developed in partnership with service users themselves, the program provided intensive, personalized support from trained mental health professionals. Crucially, it proved that people could quit safely and effectively without any disruption to their mental health. This model provides a clear, replicable blueprint, demonstrating that the tools to save lives already exist.
Implementing this blueprint requires confronting several entrenched obstacles. First, clinical attitudes must evolve. Evidence consistently shows that quitting tobacco is associated with improvements in mental well-being, including reductions in depression and anxiety, countering the outdated fear of clinical deterioration. Second, the intense nicotine dependence common in this group can be managed with adjusted support and medication. Third, the interaction between tobacco smoke and certain psychiatric drugs, which can alter medication metabolism, is a manageable clinical issue, not a reason for inaction.
Integration and equity as the path forward
A major systemic failure has been the siloed separation of mental health care from tobacco cessation services. Success depends on integration. Mental health professionals must be trained to view tobacco dependence treatment as a core part of their role. Furthermore, national tobacco control strategies must explicitly include people with mental health conditions. This includes establishing smoke-free policies in mental health facilities and ensuring access to affordable cessation aids. In lower-income countries, innovative approaches like task-shifting to lay health workers and leveraging mobile health tools offer promising, scalable solutions.
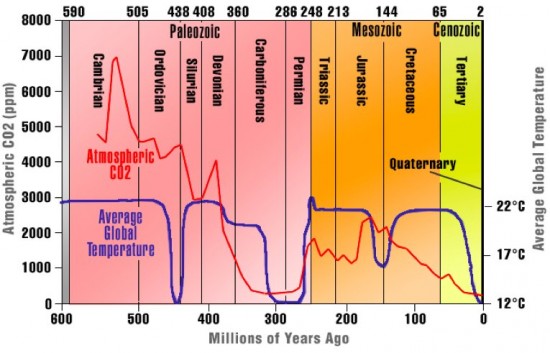
“Tobacco is deadly primarily because it severely damages the heart, tripling the risk of a heart attack and increasing the risk of dying from one by twenty-one times,” said BrightU.AI‘s Enoch. “This is largely due to carbon monoxide in the smoke, which reduces oxygen supply and weakens the heart over time. Additionally, the nicotine acts as a powerful stimulant to the autonomic nervous system, and long-term use leads to critical issues like atherosclerosis.”
The call from York is not merely for awareness but for mobilized, evidence-based action. The unseen epidemic of tobacco-related death among the mentally ill is a profound health and human rights issue. With a proven model in hand and the staggering human cost laid bare, health systems worldwide have both a moral imperative and a practical roadmap. As Professor Gilbody asserts, the life-saving tools are here. The urgent task now is to ensure they reach the hands of those who need them most, bridging a lethal gap in care that has persisted for far too long.
Watch and discover the different levels of mental health issues.
This video is from the PatchSDA channel on Brighteon.com.
Sources include:
Submit a correction >>
Tagged Under:
addiction, Brain, brain damaged, brain function, cancer, cardiovascular disease, Dangerous, epidemic, lifespan, mental health, Mind, prevention, remedies, research, smoking, stop smoking, Tobacco, tobacco-related deaths
This article may contain statements that reflect the opinion of the author